Two decades of data reveal overall increase in pain, opioid use among U.S. adults
For Immediate Release:
Wednesday, February 13, 2019
Prompted by a call from the National Academy of Medicine (formerly the Institute of Medicine) for improved national data on pain, a recent study provides new insights concerning pain trends and opioid use for pain management. Researchers used data from the Medical Expenditure Panel Survey (MEPS) to examine the impact of pain-related interference, a measure of pain’s impact on normal work activities, on people’s health status and health care use. MEPS is a nationally representative survey of the U.S. civilian, noninstitutionalized population.
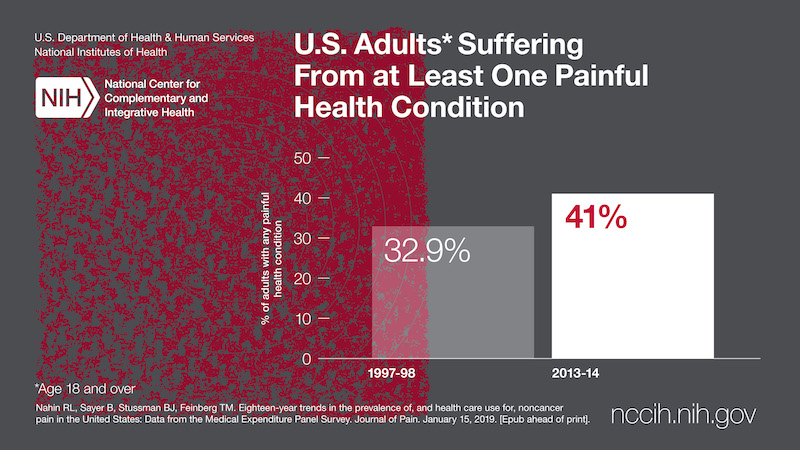
Researchers showed that the number of U.S. adults age 18 and older suffering from at least one painful health condition increased substantially from 120.2 million (32.9 percent) in 1997/1998 to 178 million (41 percent) in 2013/2014. Furthermore, the use of strong opioids, like fentanyl, morphine, and oxycodone, for pain management among adults with severe pain-related interference more than doubled from 4.1 million (11.5 percent) in 2001/2002 to 10.5 million (24.3 percent) in 2013/2014. These are the findings of a comprehensive analysis of 18-year trends showing changes in the overall rates of noncancer pain prevalence and management. The full study, conducted by the National Center for Complementary and Integrative Health (NCCIH), part of the National Institutes of Health; Social & Scientific Systems, Inc., Silver Spring, MD; and Yale University School of Medicine, New Haven, CT; was published in the Journal of Pain.
“We took a unique approach with this study by simultaneously examining long-term trends in the overall prevalence of noncancer pain in the U.S., the impact of this pain, and health care use attributable directly to pain management,” says Richard L. Nahin, Ph.D., first author on the study and NCCIH lead epidemiologist. “To address these gaps, we used data from MEPS to identify trends between 1997 and 2014.”
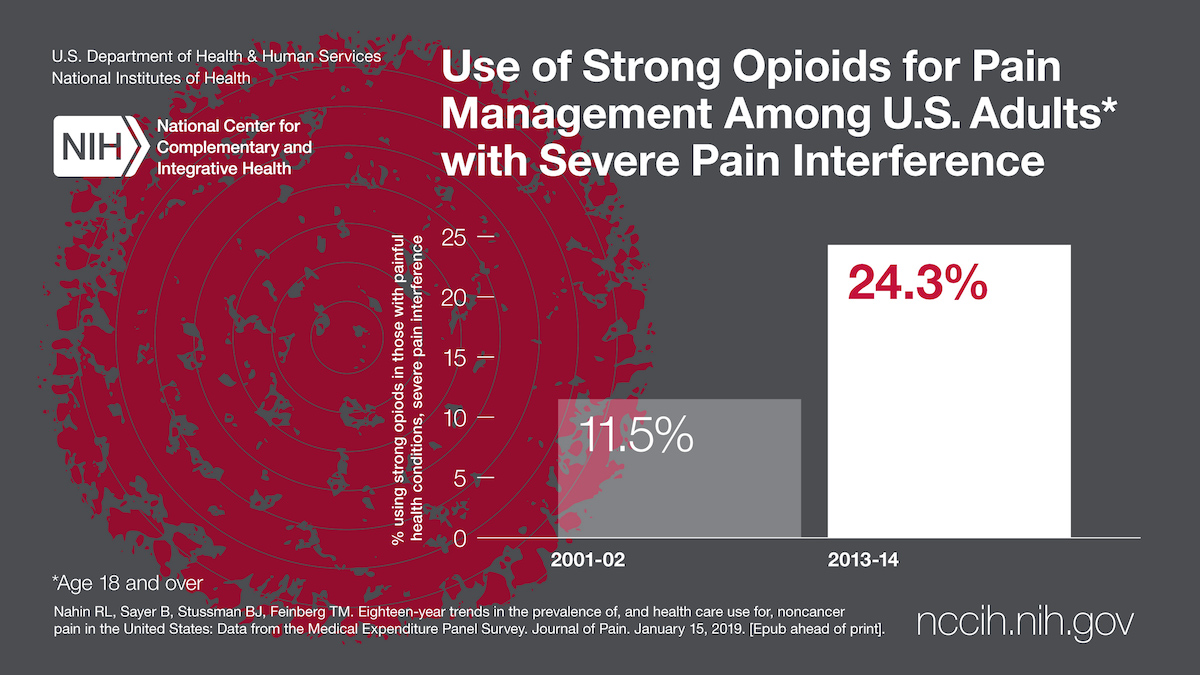
The study showed that by 2013/2014, about one-third of individuals (68 million) with a painful health condition reported moderate or severe pain-related interference with normal work activities. The analysis of MEPS data looked specifically at noncancer painful health conditions. The researchers also found that people with severe pain-related interference were more likely to use strong opioids, to have had four or more opioid prescriptions, and to have visited a doctor’s office six or more times for their pain compared to those with minimal pain-related interference.
As with other studies, this analysis showed an increase in the overall use of opioids between 1997 and 2014, with a peak use observed between 2005 and 2012. Since 2012, however, there has been a slight decrease in opioid use tied to a reduction in use of weak opioids and in the number of patients reporting only one opioid prescription.
The study also shows small changes in the prevalence of ambulatory office visits, emergency room visits, or hospitalization for pain. Ambulatory office visits for pain plateaued between 2001/2002 and 2007/2008, then decreased through 2013/2014. In addition, the researchers found a decrease in the number of pain-related emergency room visits and overnight hospital stays among those reporting at least one painful condition.
The authors noted that the study had several limitations. First, while MEPS includes comprehensive information on health conditions and types of medical care used, when surveyed, people often vary in how much they accurately remember. In addition, it is possible the survey did not capture everyone with noncancer painful health conditions. Finally, due to MEPS survey methodology and study design, direct links cannot be made between the level of pain-related interference and use of health care.
“The data show a substantial increase not only in the number of U.S. adults with painful health conditions, but also in overall use of opioids and in the number of people receiving multiple opioid prescriptions,” says Helene M. Langevin, M.D., NCCIH director. “This long-term picture of pain management is of critical importance as NIH addresses the opioid crisis. It offers insights that can help improve decision-making by stakeholders—from patients and providers to payers and policymakers.”
Reference
- Nahin RL, Sayer B, Stussman BJ, Feinberg TM. Eighteen-year trends in the prevalence of, and health care use for, noncancer pain in the United States: Data from the Medical Expenditure Panel Survey. Journal of Pain. January 15, 2019. [Epub ahead of print].
###
About the National Center for Complementary and Integrative
Health (NCCIH):
NCCIH’s mission is to define, through rigorous scientific
investigation, the usefulness and safety of complementary and
integrative health approaches and their roles in improving
health and health care. For additional information, call
NCCIH’s Clearinghouse toll free at 1-888-644-6226. Follow us
on Twitter, Facebook ,
and YouTube.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.