Federal agencies partner for military and veteran pain management research
Joint HHS-DoD-VA initiative will award multiple grants totaling $81 million
For Immediate Release:
Wednesday, September 20, 2017
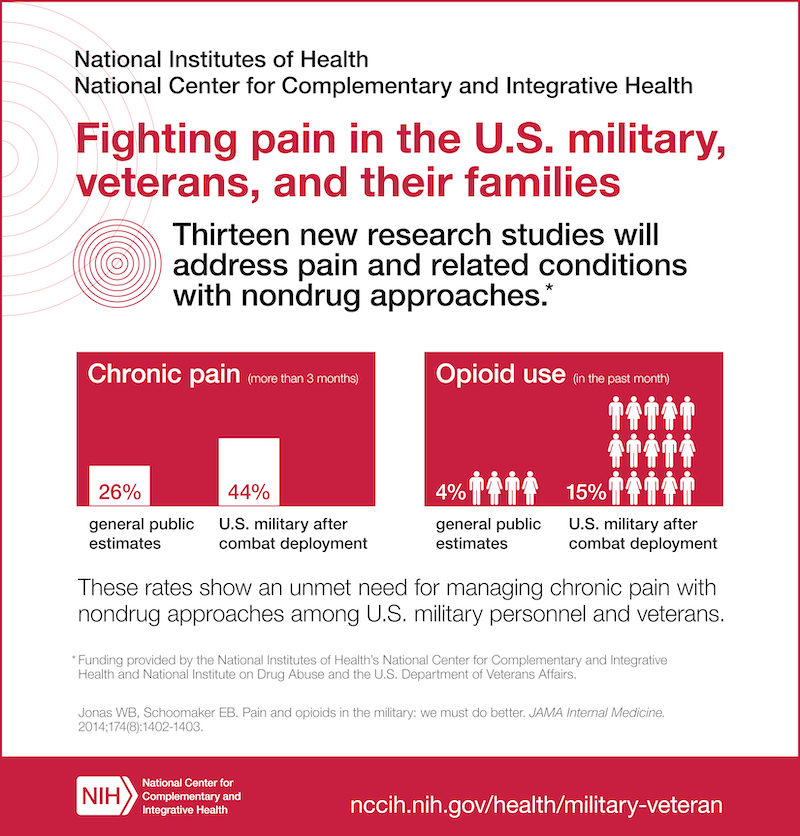
Through an interagency partnership, the U.S. Department of Health and Human Services, the U.S. Department of Defense (DoD), and the U.S. Department of Veterans Affairs (VA) announce a multi-component research project focusing on nondrug approaches for pain management addressing the needs of service members and veterans. Twelve research projects, totaling approximately $81 million over six years (pending available funds), will focus on developing, implementing, and testing cost-effective, large-scale, real-world research on nondrug approaches for pain management and related conditions in military and veteran health care delivery organizations. The National Institutes of Health (NIH) will be the lead HHS agency in this partnership.
“Finding solutions for chronic pain is of critical importance, especially for military personnel and veterans who are disproportionately affected,” said NIH Director Francis S. Collins, M.D., Ph.D. “Bringing the science to bear through these real-world research projects will accelerate our search for pain management strategies for all Americans, especially as we work to address the nation’s opioid crisis.”
These projects will provide important information about the feasibility, acceptability, safety, and effectiveness of nondrug approaches in treating pain. Types of approaches being studied include mindfulness/meditative interventions, movement interventions (e.g., structured exercise, tai chi, yoga), manual therapies (e.g., spinal manipulation, massage, acupuncture), psychological and behavioral interventions (e.g., cognitive behavioral therapy), integrative approaches that involve more than one intervention, and integrated models of multi-modal care.
The National Center for Complementary and Integrative Health (NCCIH), part of NIH, is contributing more than half of the total funding, and it is the lead for this multi-agency initiative called the NIH-DoD-VA Pain Management Collaboratory, which is modeled on the successful NIH Health Care Systems Research Collaboratory. This initiative also addresses the need to focus on “advancing better practices for pain management,” which is outlined in HHS’ 5-point strategy to combat the opioid crisis.
“NCCIH has made pain research a priority—especially in military and veteran populations. We first partnered with the National Institute on Drug Abuse and the VA in 2014 and are delighted to expand the partnership to include the DoD and additional HHS/NIH components,” said Dr. Josephine Briggs, director of NCCIH.
“We are so pleased to work alongside our federal partners to develop effective ways to treat pain in our service members and veterans that do not expose them to the risks of opioids,” said Rachel Ramoni, D.M.D., Sc.D., chief research and development officer for the VA. “This work reflects the VA’s commitment to reducing opioid overuse and expanding alternative pain management.”
Studies report nearly 45 percent of soldiers and 50 percent of veterans experience pain on a regular basis, and there is significant overlap among chronic pain, post-traumatic stress disorder (PTSD), and persistent post-concussive symptoms. Data from the National Health Interview Survey shows that American veterans experience a higher prevalence of pain and more severe pain than nonveterans. Although opioids are often prescribed to treat chronic pain, research has not shown them to be very effective, and there are many issues with long-term use. Thus, there is a need for nondrug approaches to complement current strategies for pain management and to reduce the need for, and hazards of, excessive reliance on opioids.
“Pain is the most common medical condition requiring treatment for military personnel. Current drug treatments have limited efficacy and are often associated with severe adverse events, significant cognitive and physiological side effects, and pose a significant risk of abuse, misuse, addiction, tolerance, and diversion. The proposals funded under this interagency partnership will provide a significant step forward in pain management in our wounded service members. We are pleased to be working with our interagency partners in driving changes to clinical practice that will impact the military, our veterans, and the Nation as a whole,” said Dr. George Ludwig, principal assistant for research and technology, U.S. Army Medical Research and Materiel Command (USAMRMC).
Seven of the 12 projects have been awarded by HHS/NIH. The remaining five will be announced by the DoD and VA in the coming months. The HHS/NIH awarded institutions are:
- Robert Kerns, Ph.D., Yale University, New Haven, Connecticut. Dr. Kerns and his team, in collaboration with their VA, DoD, and Yale partners, will establish the Pain Management Collaboratory Coordinating Center. This center will provide national leadership and serve as a national resource for development and refinement of innovative tools, best practices, and other resources in the conduct of high impact pragmatic clinical trials on nondrug approaches for pain management and other comorbid conditions in veteran and military health care systems. They will use their expertise in pain management, electronic health records, data systems, and the design and coordination of multi-site real-world trials to support the design and implementation of the pragmatic trials funded through this initiative. (Funded by NCCIH, ORWH, NINDS, OBSSR)
- Julie Fritz, Ph.D., University of Utah, Salt Lake City. This project will research a stepped care approach for the treatment of low-back pain. Stepped care is a treatment process that begins with broadly accessible, less intensive interventions that can benefit many patients. Those who do not respond to initial treatments are stepped up to receive more intensive treatment. (Funded by NCCIH)
- Karen Seal, M.D., Northern California Institute for Research and Education, San Francisco. The overarching goal of this demonstration project is to implement a new Whole Health model for chronic pain care, emphasizing nondrug pain self-management that reduces pain symptoms and improves overall functioning and quality of life in veterans. (Funded by NCCIH, NICHD)
- Alicia Heapy, Ph.D., Yale University, New Haven, Connecticut. The overall goal of this project is to conduct a pragmatic trial to examine the real-world effectiveness of an interactive voice response-based form of cognitive behavioral therapy for chronic pain called COoperative Pain Education and Self-management. (Funded by NCCIH, NINR, NIAAA)
- Christine Goertz, D.C., Ph.D., Palmer College of Chiropractic, Davenport, Iowa. The researchers will develop and implement a pragmatic randomized trial that looks at the effects of different doses and maintenance of chiropractic care for low-back pain. (Funded by NCCIH, ORWH)
- Steven George, Ph.D., Duke University, Durham, North Carolina. The goal of this planning and demonstration project is to improve access to recommended nondrug therapies for low-back pain in the Department of VA Health Care System. (Funded by NCCIH)
- Marc Rosen, M.D., Yale University, New Haven, Connecticut. This research will test the effectiveness and cost-effectiveness of Screening, Brief Intervention, and Referral to Treatment for Pain Management, designed to reduce pain and risky substance use. (Funded by NCCIH, NIDA)
HHS/NIH co-funders include the National Institute on Drug Abuse, National Institute on Alcohol Abuse and Alcoholism, National Institute of Neurological Disorders and Stroke, National Center for Medical Rehabilitation Research, which is part of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Nursing Research, Office of Research on Women’s Health, and Office of Behavioral and Social Sciences Research. The DoD is funding this initiative through its Clinical and Rehabilitative Medicine Research Program and Military Operational Medicine Research Program, and the VA is providing funding through VA Office of Research and Development.
###
About the National Center for Complementary and Integrative Health (NCCIH):
NCCIH’s mission is to define, through rigorous scientific investigation, the usefulness and safety of complementary and integrative health approaches and their roles in improving health and health care. For additional information, call NCCIH’s Clearinghouse toll free at 1-888-644-6226. Follow us on Twitter, Facebook , and YouTube.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit nih.gov.