Director’s Message

This unprecedented year has been a reminder of the importance of rigorous scientific investigation in ensuring and promoting human health. COVID-19 may be the first major pandemic we have seen in our lifetimes, but Americans have been facing the realities of “noncommunicable epidemics” for some time–opioid abuse, chronic pain, obesity, diabetes, and suicide. These persistent and related public health crises underline the systemic challenges we must recognize and take on if we are to improve our society’s overall state of health. Multiple chronic conditions in individuals, such as obesity, diabetes, cardiovascular disease, and degenerative joint disease, are not only comorbid with chronic pain, depression, opioid addiction, and suicide but also share common contributing factors such as poor diet, sedentary lifestyle, environmental exposures, and chronic stress–often the consequences of poverty and food and housing insecurity. The domino effect of chronic conditions is seen in the disproportionate toll they take on Latino, Black, American Indian, Alaska Native, and other communities that are often underserved in our health care ecosystem. We have certainly witnessed the dire consequences of these effects during the COVID-19 pandemic, which illustrates how chronic underlying conditions pose immediate and long-term risks to those infected.
Now, more than ever, we need to look at the multiple factors that promote either health or disease and scientifically consider the whole person as a complex system in which health and disease are part of a bidirectional continuum. Our current biomedical research model is superb in advancing the diagnosis and pharmacologic treatment of organ-specific diseases with growing precision. This knowledge is based on an increasingly sophisticated understanding of pathogenesis, or the mechanisms by which diseases occur. On the other hand, health restoration through self-care, lifestyle, or behavioral interventions is much less studied. Examples of health restoration, or “salutogenesis,” would be the return to health after an acute viral illness or flareup of a chronic condition; normalization of cholesterol, hemoglobin A1C, and/or blood pressure in a patient with metabolic syndrome through lifestyle modification; and return to function and mobility following a musculoskeletal injury. We currently do not know whether salutogenesis consists of “pathogenesis in reverse” or whether it requires some specific salutogenic or healing pathways to be engaged to bring an individual back toward health. Unlike the treatment of disease with drugs that target specific molecular pathways, health restoration through salutogenesis is likely complex and multifactorial and involves the whole person. Advancing research on whole person health will support the investigation of nondrug and noninvasive approaches to improve and restore health.
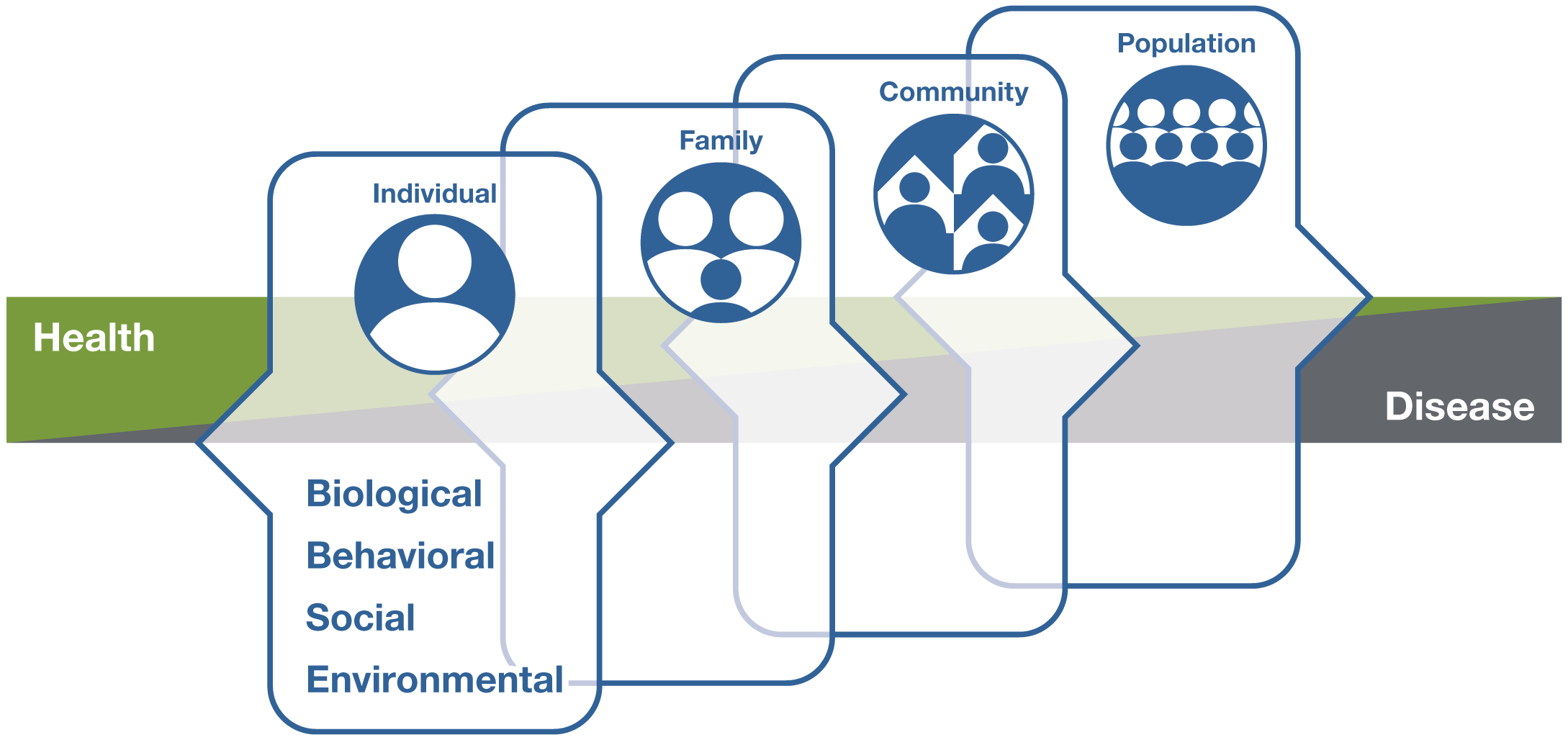
Meeting this challenge is right up our alley. By its nature, the mission of NCCIH includes both integration and health. NCCIH was created more than 20 years ago to facilitate the study and evaluation of complementary and alternative medical practices and to disseminate the resulting information to the public. Over time, we incorporated a focus on integrative health research to bring conventional and complementary approaches together in a safe, coordinated way with the goal of improving clinical care for patients, promoting health, and preventing disease. Now, we are expanding our definition of integrative health to include whole person health, or empowering individuals, families, communities, and populations to improve their health in multiple interconnected domains: biological, behavioral, social, and environmental. This strategic plan, built on the foundation NCCIH has fostered for two decades, continues to advance our mission through an effort to better define and map a path to whole person health. We will do this by building on current activities and existing collaborations with other NIH Institutes, Centers, and Offices while advancing new strategies and ideas. The objectives and strategies listed here will also be considered through the lens of minority health and health disparities, such that the knowledge they generate is inclusive of populations with the greatest needs.
The objectives and strategies presented in this 5-year plan reflect our continued commitment to advancing fundamental science and methods development for both basic and clinical research. We also present strategies to advance research on whole person health and the integration of complementary and conventional care. And with the goal of improving and restoring health rather than just treating disease, we offer strategies to foster research on health promotion and restoration, resilience, disease prevention, and symptom management. As always, we remain committed to enhancing the complementary and integrative health research workforce and disseminating what we learn.
From April 2020 through July 2020, we offered stakeholders several ways to contribute their thoughts and feedback on this plan. This included responding to a request for information RFI using a web form or by email. The Center broadly disseminated information throughout the process to its many stakeholder groups and individuals. In May 2020, we hosted the webinar and town hall Whole Person Health: Mapping a Strategic Vision for NCCIH in conjunction with the International Congress on Integrative Medicine and Health. In July 2020, a Center-hosted Town Hall and Public Comment Session invited comments from stakeholders, experts, communities, and members of the public, including but not limited to researchers and trainees across academia, industry, and government; health care providers and health advocacy organizations; nongovernmental, scientific, and professional organizations; and Federal agencies.
The draft strategic plan was posted to the NCCIH website in February 2021, and an RFI was issued for public comment on the draft (https://grants.nih.gov/grants/guide/notice-files/NOT-AT-21-005.html). The National Advisory Council for Complementary and Integrative Health provided input into the strategic planning process and received updates during its public sessions in September 2019; February, June, and September 2020; and January 2021.
As director of the Center, I am confident that our diligence in hearing from a diverse group of stakeholders has helped us develop a set of research priorities guided by attention to public health needs, scientific promise, amenability of topics to rigorous scientific inquiry, potential to impact health care practices, and relationship to use and practice. We know that priorities can change–2020 certainly taught us that–so we must always have our ears to the ground and our eyes on the sky. Priorities and innovation can come through investigator-initiated applications as well as from programmatically directed funding initiatives. We must always be agile and responsive to challenges and opportunities that come our way.
Much progress has been made in the research areas that form the NCCIH portfolio since our last strategic plan was released, but there is still much to do. As we look forward to the next 5 years, we will continuously think strategically about existing programs and priorities, the growing evidence base, research capacity, scientific opportunities, and public health needs.