Building a Path to Whole Person Health
Whole person health is not altogether a new goal. A whole person health perspective has been central to NCCIH’s mission dating back to its origins. The Center’s current definition of “integrative health” refers to treatment of the whole person as opposed to separate organ systems. Integrative health also aims for well-coordinated care among different providers and institutions by bringing conventional and complementary approaches together to care for the whole person. Further, one of the Center’s longstanding strategic objectives is to foster health promotion and disease prevention, central tenets of whole person health.
This strategic plan has been informed and shaped by an effort to better define and map a path to whole person health by expanding and building on current activities while advancing new research strategies and ideas to promote its realization. The concept of whole person health will continue to evolve, just as the concept of complementary medicine has changed over time as the line between conventional and complementary medicine has increasingly become blurred.
What Is Whole Person Health?
Whole person health is a concept and a vision as well as an organizing principle. There are many ways to promote and achieve it, and methods and strategies will evolve as understanding and refinement of this concept mature over time.
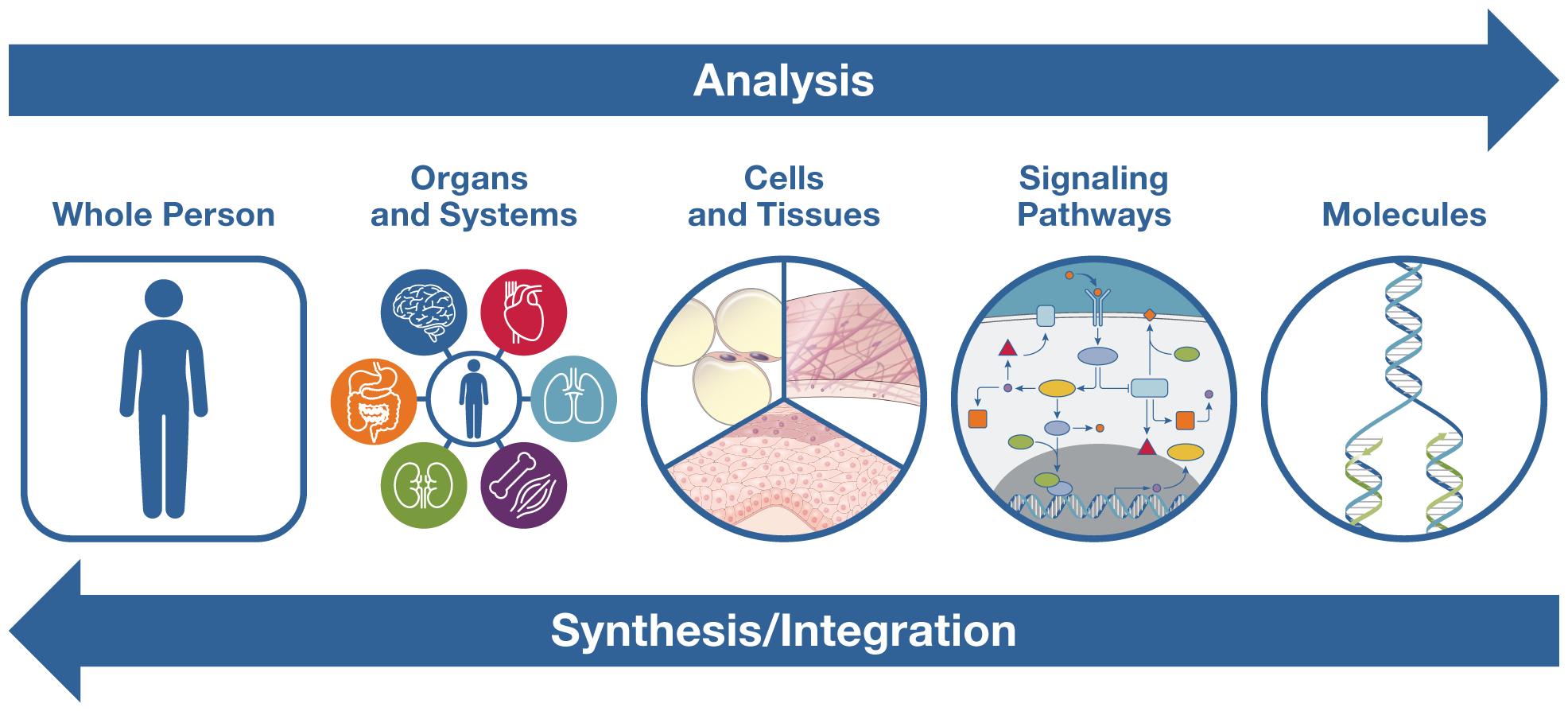
Any kind of knowledge base includes both analysis and synthesis: analysis breaks things down into individual components, and synthesis puts them back together to understand the whole. For more than a century, biomedicine has been strongly pulled toward analysis, from its early organization into organ systems in the late nineteenth century to cellular and molecular biology with its increasingly detailed understanding of cells, molecules, genetics, and signaling pathways. In the last few decades, systems biology, derived from ecology, has begun to influence biomedical research, with a greater awareness of how body systems relate to one another and how networks of genes influence physiological processes. Nevertheless, our predominantly biochemical approach to treatment remains overwhelmingly pharmacologic. And because we tend to think about a specific disease or specific organ system, even when co-occurring conditions are present, we typically treat them separately, sometimes with medications that interfere with one another.
Now is the time for biomedical science to work toward restoring its balance between analysis and synthesis. We can do this by strengthening our efforts toward integration of knowledge across disciplines, focusing on the whole person, and taking a transdisciplinary approach that integrates the natural, social, and health sciences and transcends traditional boundaries.
We also need to recognize that health and disease are not separate disconnected states but rather a bidirectional continuum. We know that on the path between health and disease, some unhealthy behaviors, such as poor diet, sedentary lifestyle, chronic stress, and poor sleep, as well as social determinants of health (the conditions in which people are born, grow, live, work, and age) can lead to chronic diseases of multiple organ systems, such as diabetes, cardiovascular disease, degenerative joint disease, and depression. Addressing these issues at an early stage can not only prevent multiple diseases but also restore health and stop progression to disease across the lifespan. We witnessed this in real time in 2020 and 2021. Although COVID-19 is a respiratory infection, chronic conditions in other body systems (e.g., diabetes, hypertension) as well as social determinants of health are important factors in its severity and mortality.
By looking at the entire health/disease spectrum in a bidirectional way, we can expand our understanding of integrative health to include the return to an improved state of health, in addition to disease prevention. By looking at connections across biological, behavioral, social, and environmental domains, we can better understand how co-occurring conditions can arise from common, interrelated factors. As a result, we can also examine the potential role of multicomponent behavioral and/or systems-level interventions in addressing these problems and restoring health. It is possible that one intervention developed with the whole person in mind could cross several systems, restoring health in all.
Integrated Approach to Multisystem Health Restoration

How To Study Whole Person Health?
Research on whole person health aims to identify the gaps in our knowledge of the progression from health to disease and from disease back to health. It also may identify gaps in integration of care to develop multicomponent interventions that not only prevent progression to disease but also restore an improved state of health, as well as systems-level interventions to improve access to and/or reimbursement for these interventions. In addition, complementary health approaches such as yoga, mindfulness meditation, and tai chi impact multiple systems of the body (e.g., respiratory, neural, and musculoskeletal). This makes thinking about health in terms of the whole person important to understanding the role of complementary approaches in promoting health and preventing disease.
Strategic plans in the early history of the Center expressed an interest in exploring many paths, including research on systems of care such as traditional Chinese medicine, Ayurveda, and naturopathy. This type of research is challenging to conduct, and there were many stumbling blocks along the way. Figuring out the right methods for studying complex interventions was perplexing. As a result, many of the studies did not bear fruit.
In subsequent years, there was a concerted effort to address this problem by focusing on specific strategically chosen areas, such as natural products and mind and body therapies. There was also a decision to focus on symptom management, especially for pain, anxiety, and depression, which are some of the main reasons driving the use of complementary therapies. NCCIH also supported methods development for both basic science and clinical trials. The development of methodologies for conducting rigorous pragmatic trials was particularly important and will be invaluable for conducting research on whole person health.
First Steps
As part of the strategic planning process, NCCIH has been examining the meaning of the terms complementary, integrative, and health in the Center’s name and has transitioned to more inclusive definitions to reflect a whole person approach, considering:
- The growing understanding of the overlap of complementary approaches with the conventional nutritional, psychological, and physical categories.
- The increased interest in various types of synthesis or integration in biomedical science, such as systems biology and integrative physiology.
- The recognition of common risk factors for a broad range of co-occurring conditions.
A whole person health framework also provides critical insights and opportunities to expand and build on NCCIH’s current research portfolio on natural products and mind and body approaches. By deepening our scientific understanding of the connections that exist across domains of human health, we can better understand how conditions interrelate, define multicomponent interventions that address these problems, and expand how we support patients through the full continuum of their health experience, including the return to health.